An 84-year-old patient was admitted to hospital for decompensation of chronic heart failure with worsening dyspnea (present at rest at the moment). An acute coronary syndrome was excluded, diuretic therapy without significant response. The patient underwent pleural puncture on the right side two days ago (approximately 2000 ml of transudate were evacuated).
The patient was admitted to ICU for renal replacement therapy to reach a negative fluid balance.
The patient already suffered only from mild dyspnea at rest. No pain was present. The patient was haemodynamically stable without the necessity of catecholamine support. Blood pressure 114/60 mmHg, 90 bpm, atrial fibrillation, capillary refill time below 2 seconds. Auscultation revealed clear, silent breath sounds. No breathing sounds could be heard basally bilaterally. Perimalleolar and calf oedema bilaterally. Anasarca of dorsal parts of both thighs, arms and trunk. Lab results did not reveal increased levels of lactate. Anuria due to established continuous veno-venous haemodialysis.
Patient´s history encompasses chronic heart failure with several decompensations in the past, arterial hypertension, state after deep vein thrombosis and B-cell lymphoma (watch and wait strategy). The patient has single-chamber pacemaker with a stimulating electrode inserted into right ventricular apex due to atrial fibrillation with a slow ventricular response.
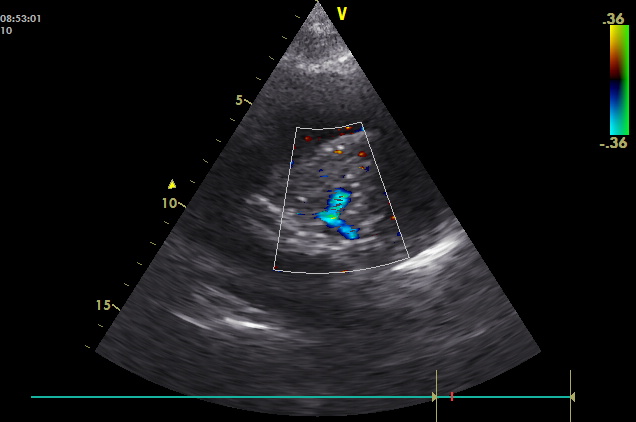
Lung ultrasonography and echocardiography:
<h3>
