You are called to the emergency department. An ambulance brought an 85-year-old patient after successful CPR.
The patient was recently discharged from the department of internal medicine. He was hospitalised for pneumonia, received antibiotic therapy and was discharged in good health condition. On the discharge day already at home, his family found him in the shower – he was unconscious and not breathing. The ambulance was called, T-CPR was not performed. Asystole was seen on the monitor. After 30 minutes of CPR, the heart rhythm was restored – ventricular rhythm, HR 20-40 bpm, pulse was palpable over the large vessels. Heparin 5000 IU and aspirin 500 mg i.v. were administered. Under intermittent administration of 1 mg of adrenalin every 2 minutes, the patient was transported to the closest hospital (to you).
The Patient has a history of severe coronary artery disease with several interventions in the past. During hospitalisation for pneumonia, dual antiplatelet therapy was reduced to monotherapy with aspirin. Further known comorbidities are pulmonary fibrosis, hypercholesterolemia and chronic cor pulmonale with cardiac cirrhosis. The last ECG (at the department of internal medicine) was described as sinus rhythm without any block.
During admission: cyanosis, dilation of pupils without reaction to light stimulation, GCS 3, pulse over the large arteries is palpable with a deficit in peripheral parts (peripherally are palpable only approximately 10 bpm). Auscultation reveals clear, very silent breathing sounds without pathological phenomena. The abdomen is soft, and limbs are cyanotic, cold and without oedema. Intraosseous access was established.
Administration of adrenalin continuous via the intraosseous access. A peripheral venous catheter was inserted. Blood was taken for lab tests.
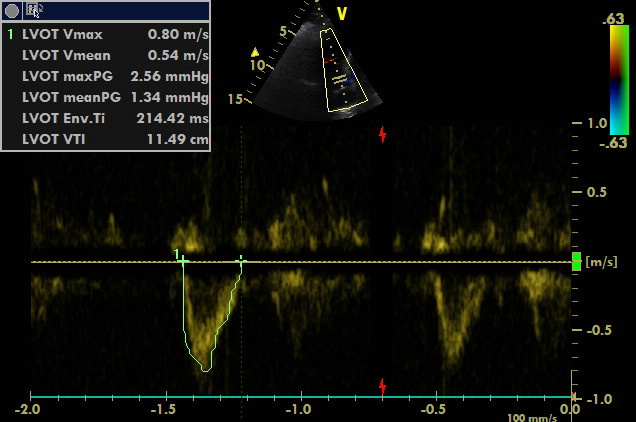
Echocardiography was performed simultaneously with the following findings: Left ventricle is small without significant RWMA unless the dysfunctional septum. The right ventricle is dilated and dysfunctional with D-shaped interventricular septum, dilation of VCI and hepatic veins. ECG shows ventricular rhythm and RBBB.
Thrombolysis was administered. Heart rate increased to 80 bpm, and pulse deficit disappeared. Artery line was established, IABP monitoring started, and the patient was transferred to the ICU.
Ultrasonography was performed at the ICU:
