A 69-year-old man with a history of chronic ischemic heart disease, myocardial infarction and chronic heart failure. He underwent implantation of CRT (biventricular cardiac resynchronisation stimulation therapy) one year ago. Now the patient was admitted to the department of internal medicine for worsening dyspnea. Coronarography revealed the diffuse 3-vessels disease. The finding did not require intervention. Health condition of the patient worsened the next day with confusion by incoming sepsis. Intubation was necessary due to respiratory failure.
The patient received analgosedation and mechanical ventilation (BiPAP, Pmax 24, PEEP 10, FiO2 50% and tidal volume around 450 ml), support of circulation by the administration of noradrenaline 2.4 mg/h, adrenaline 0.5 mg/h and vasopressin 1 IU/h. Blood pressure was 120/60 mmHg. ECG revealed heart rate 120 bpm by irregular spontaneous rhythm without P waves and wide QRS complexes (atrial fibrillation with left bundle branch block). Diuresis was preserved, capillary refill time around 2s, without peripheral oedema. Auscultation revealed very silent breathing sounds bilaterally, on the left side ventrally almost inaudible, dorsobasally inspiratory crackles with restricted breathing. The abdomen was difficult to examine by palpation, but without signs of peritoneal irritation. Peristalsis was inaudible. A cooling catheter was inserted into inferior vena cava via the femoral vein due to core body temperature exceeding 42 °C. The goal temperature was set to 37.4 °C.
PiCCO measurement was initiated: stroke volume 40 ml, GEDVI 1169, ELWI 16, dP/dT 840, stroke volume variation was not assessed due to the presence of atrial fibrillation, SVRI 1000. Thermodilution fluid to calibration was administered into inferior vena cava via the venous lumen of the cooling catheter.
Lab results revealed high inflammatory markers: neutrophilic leucocytosis 22000/ul, procalcitonin 12 ng/l, CRP 340 mg/l, lactate 1.7 mmol/l, positive base excess.
Several questions are arising. Is the dosage of catecholamines, vasopressin and fluids titrated well? Do we already have a septic focus (which is expected to be in the lungs) under control? Is iatrogenic complication possible? Physical examination, lab results and symptoms indicate that perfusion of the organs seems to be sufficient at the cost of enormous pharmacological support.
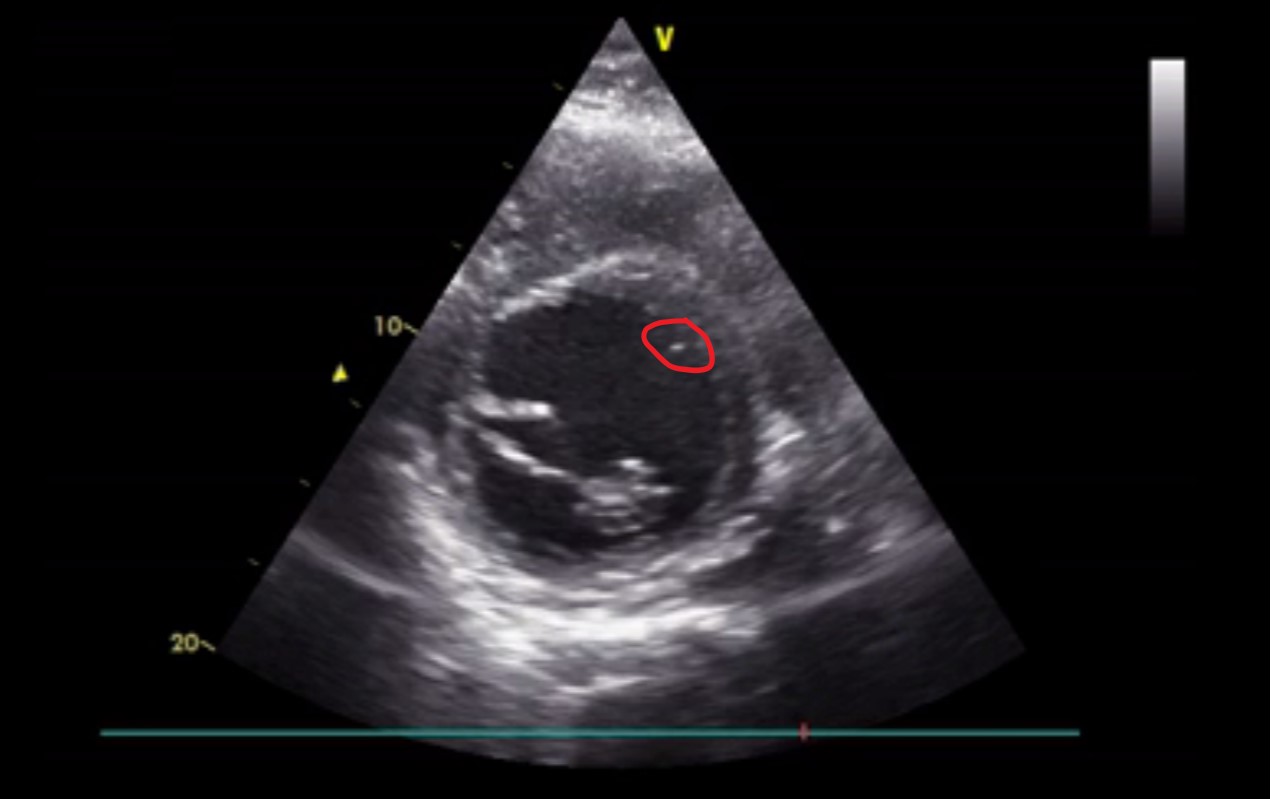
Bed-side ultrasonography:
