A 91-year-old patient with a history of hypertension and osteoarthrosis visited the ED because of worsening of abdominal pain in the past two days. Pneumoperitoneum was revealed. By surgical revision, perforated gastric ulcer was found and Billroth-II resection performed. After the surgery, she was transferred to the ICU and extubated without any problem on the 2nd day.
Noradrenaline 0.26 ug/kg/min, blood pressure 100/35/57 mmHg, the periphery is cold, capillary refill time around 1 second, normal lactate and base excess, diuresis 0.5 – 1 ml/kg/h with continual administration of furosemide.
Borderline blood pressure in a patient with a history of hypertension treated with triple combination antihypertensive therapy. Borderline diuresis and peripheral blood supply. During the ward round, we considered administering either fluid or inotropes to reduce the dose of noradrenaline and improve perfusion.
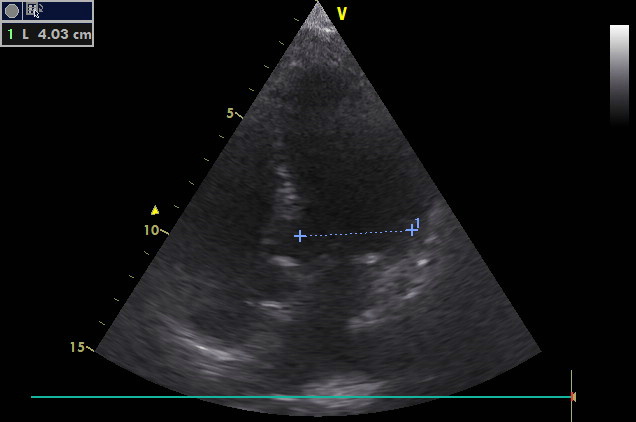
The examination starts at BLUE points bilaterally in order not to miss eventual pneumothorax as an obstructive component of the shock. At the same time, lung hydration status can be obtained with a question, whether subclinical interstitial pulmonary oedema is present or not, which may be a contraindication for further volume therapy (see, e.g. FALLS protocol):
